On July 12, the Centers for Medicare & Medicaid Services (CMS) published its 2019 Medicare Physician Fee Schedule Proposed Rule (Proposed Rule) covering a wide range of topics. In our series of articles, we have summarized and offered our insights on several key provisions. Note that comments on the Proposed Rule were due to CMS by September 10, 2018, and we expect CMS to publish the Final Rule later this fall. Of the 15,313 comments CMS received on the Proposed Rule, 1,212 of them included the acronym MIPS. You can review all the comments here.
In the Proposed Rule, CMS explains that “[i]n the years since 2012, we have acknowledged the shift in medical practice away from an episodic treatment-based approach to one that involves comprehensive patient-centered care management, and have taken steps through rulemaking to better reflect that approach in payment under the [Medicare Physician Fee Schedule].” Consistent with this philosophy, CMS continues its march forward in the 2019 Proposed Rule, including new reimbursement for a wide range of non-face-to-face services.
Medicare Telehealth Services
Each year, CMS considers whether to expand the list of Medicare-covered telehealth services, i.e., those telehealth services for which payment is made only if furnished to a beneficiary located in certain types of originating sites. For 2019, CMS proposes to expand eligible covered services to include prolonged preventive services (HCPCS G0513 and G0514).
CMS also goes to great lengths to clarify the difference between Medicare telehealth services, which are limited by the geographic and site-of-service restrictions found in section 1834(m) of the Social Security Act, and other services generally described as “telehealth.” The former, CMS notes, refers to “a discrete set of physicians’ services that ordinarily involve, and are defined, coded, and paid for as if they were furnished during an in-person encounter between a patient and a healthcare professional.”
By contrast, the latter refers to “services that are defined by and inherently involve the use of communication technology.” These services, CMS explains, are not subject to the section 1834(m) restrictions, and therefore may be reimbursable without regard to the patient’s location.
For years, telehealth advocates have bemoaned the section 1834(m) restrictions as stunting the growth of telehealth and urged CMS to waive its requirements with respect to certain services. CMS now has done one better, concluding the restrictions do not apply unless the service is one which traditionally has been furnished face-to-face. As a result, CMS now proposes new reimbursement for remote patient monitoring (RPM), virtual check-ins, and interprofessional internet consultations.
Remote Patient Monitoring
In 2018, CMS began reimbursing for RPM under CPT® 99091.[1] In a recent white paper, we detailed the billing requirements for this code. For 2019, CMS proposes adding three new RPM codes:
CPT® 990X0: Remote monitoring of physiologic parameter(s) (e.g., weight, blood pressure, pulse oximetry, respiratory flow rate), initial; set-up and patient education on use of equipment.
CPT® 990X1: Remote monitoring of physiologic parameter(s) (e.g., weight, blood pressure, pulse oximetry, respiratory flow rate), initial; device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days.
CPT® 994X9: Remote physiologic monitoring treatment management services, 20 minutes or more of clinical staff/physician/other qualified healthcare professional time in a calendar month requiring interactive communication with the patient/caregiver during the month.
The first two codes are reimbursement for the practice expense associated with furnishing RPM services; no physician work is required to bill for either code. The proposed reimbursement for CPT® 990X0 is approximately $21, and $69 for CPT® 990X1.
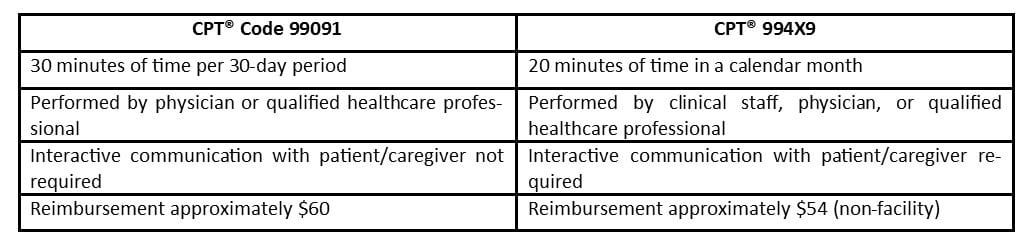
CPT® 994X9 offers an alternative to—not a replacement for—billing CPT® 99091 for professional services associated with RPM. The following illustrates the differences between the two codes:
CMS provides no detail in the Proposed Rule regarding the billing requirements for the three new RPM codes beyond the code descriptions quoted above, leaving many unanswered questions. For example, what level of supervision is required for clinical staff under CPT® 994X9? What constitutes “interactive communication with the patient/caregiver?” Hopefully, through the comments it receives on this proposal, CMS will identify and address these issues, giving providers greater confidence as they develop and expand RPM programs.
Virtual Check-In
Presently, CMS has not made separate payment to physicians for brief check-in services furnished using communication technology to evaluate whether an office visit or other service is warranted. If the physician decides to see the patient, CMS considers the check-in bundled into the payment for the resulting visit. If, however, the check-in does not lead to an office visit, the physician goes without payment for the time and effort associated with the check-in.
In the Proposed Rule, CMS acknowledges the problems this reimbursement model creates:
To the extent that these kinds of check-ins become more effective at addressing patient concerns and needs using evolving technology, we believe that the overall payment implications of considering the services to be broadly bundled becomes more problematic. Effectively, the better practitioners are in leveraging technology to furnish effective check-ins that mitigate the need for potentially unnecessary office visits, the fewer billable services they furnish. Given the evolving technological landscape, we believe this creates incentives that are inconsistent with current trends in medical practice and potentially undermines payment accuracy.
To address this, CMS proposes to pay for check-in services under HCPCS code GVCI1. The reimbursable service is narrowly defined:
Brief communication technology-based service, e.g. virtual check-in, by a physician or other qualified healthcare professional who can report evaluation and management [E/M] services, provided to an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion.
CMS proposes to pay approximately $15 for this service based on the low work time and intensity and to account for the resource costs and efficiencies associated with the use of communication technology.
CMS also proposes to make separate payment when a physician uses recorded video and/or images captured by a patient under another new code, HCPCS GRAS1. This reimbursable service also is narrowly defined:
Remote evaluation of recorded video and/or images submitted by the patient (e.g., store and forward), including interpretation with verbal follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment.
CMS proposes to pay approximately $13 for this service.
Although it proposes to move forward with new reimbursement for virtual check-ins, CMS seeks comment on how to prevent billing abuses. Specifically, CMS asks whether there should be frequency limits on these check-ins, whether the proposed time periods for bundling the service (i.e., 7 days and 24 hours) are appropriate, and whether providers should be required to secure consent from the patient or caregiver. Also, with respect to GRAS1, CMS seeks comment on whether the service may be offered to new patients.
Interprofessional Internet Consultation
Because specialists receive no reimbursement for time spent consulting with treating practitioners regarding specific patients, specialist input often requires scheduling a separate patient visit when telephonic or internet-based interaction between the specialist and the treating practitioner would suffice. To address this, CMS proposes new reimbursement for interprofessional consultations under six codes:
CPT® 994X6: Interprofessional telephone/internet/electronic health record assessment and management service provided by a consultative physician including a written report to the patient’s treating/requesting physician or other qualified healthcare professional, 5 or more minutes of medical consultative time (reimbursement approximately $27).
CPT® 994X0: Interprofessional telephone/internet/electronic health record referral service(s) provided by a treating/requesting physician or qualified healthcare professional, 30 minutes (reimbursement approximately $27).
CPT® 99446: Interprofessional telephone/internet assessment and management service provided by a consultative physician including a verbal and written report to the patient’s treating/requesting physician or other qualified healthcare professional; 5-10 minutes of medical consultative discussion and review (reimbursement approximately $18).
CPT® 99447: Same as CPT® 99446, except 11-20 minutes (reimbursement approximately $36).
CPT® 99448: Same as CPT® 99446, except 21–30 minutes (reimbursement approximately $54).
CPT® 99449: Same as CPT® 99446, except 31 or more minutes (reimbursement approximately $73).
CMS explains this reimbursement is not intended for activities undertaken for the benefit of the practitioner, such as information shared as a professional courtesy or as continuing education. Also, because these codes concern services furnished without the beneficiary present, CMS proposes to require the treating practitioner to obtain and document verbal beneficiary consent prior to the provision of services.
Chronic Care Management
Presently, there are three codes under which a practitioner may bill for chronic care management: CPT® 99490, CPT® 99487, and CPT® 99489. Each of these codes reimburses for time spent by clinical staff furnishing care management services under the general supervision of a physician or other qualified healthcare professional.
CMS now proposes to reimburse for care management services personally provided by a physician or other qualified healthcare professional under CPT® 994X7. The billing requirements for this new code are otherwise the same as CPT® 99490, except CPT® 994X7 requires a minimum of 30 minutes of services over a calendar month. CMS’ proposed reimbursement for CPT® 994X7 is appropriately $74, compared to approximately $43 for CPT® 99490.
Bundled Episode of Care for Management and Counseling Treatment for Substance Abuse Disorders
Noting “[t]here is an evidence base that suggests that routine counseling, either associated with medication assisted treatment (MAT) or on its own, can increase the effectiveness of treatment for substance use disorders (SUDs),” CMS seeks comment regarding separate payment for a bundled episode of care for management and counseling for SUDs. The agency does not offer any specific proposal to which to react; instead, CMS asks for stakeholder feedback regarding how to define and value the bundle and what conditions of payment should be attached.
CMS’ proposal to make a single payment for a specific bundle of care management services for beneficiaries with SUDs differs from the approach CMS has taken with care management services for beneficiaries with chronic conditions. With regard to the latter, CMS has given providers broad latitude in developing and implementing individual care plans, paying them based on the amount of time devoted to these activities. In the context of SUDs, however, CMS is considering a more prescriptive approach, paying providers based on providing a defined scope of services over a specified time period.
PYA assists organizations in defining and developing telehealth strategies and performs valuations of telehealth arrangements. For more information, contact one of our PYA executives below at (800) 270-9629.
[1] Current Procedural Terminology (CPT®) is a registered trademark of the American Medical Association.
© 2018 PYA
No portion of this article may be used or duplicated by any person or entity for any purpose without the express written permission of PYA.


